Home » Services » Interventional procedures » Endovascular Treatment for Carotid Arteries
Endovascular treatment for carotid arteries
What are cardotid arteries?
Arteries carry oxygen-rich blood from the heart to the head and body. There are two carotid arteries (one on each side of the neck) that supply blood to the brain. The carotid arteries are palpated on each side in the lower part of the neck, just below the angle of the jaw.
The carotid arteries bring blood to the large, frontal part of the brain, which is responsible for thinking, speech, personality, and sensory and motor functions.
The vertebral arteries pass through the spine and bring blood to the back of the brain (brain stem and cerebellum).
Carotid artery disease – carotid artery stenosis
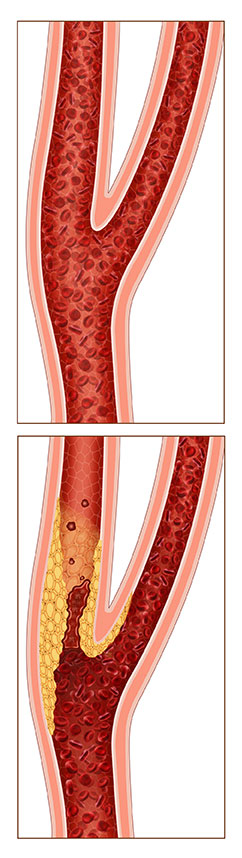
Carotid artery disease, also called carotid artery stenosis, is a narrowing of the carotid arteries, usually caused by atherosclerosis. Atherosclerosis is the accumulation of cholesterol, fats and other substances that travel through the bloodstream, such as inflammatory cells, cell waste products, protein and calcium. Over time, these substances stick to the walls of blood vessels as people age and combine to form a material called plaque.
Plaque buildup can lead to narrowing or blockage of the carotid artery, which can lead to an increased risk of stroke.
Sometimes the narrowing of the blood vessels of the neck can be a consequence of radiation therapy of the neck or after surgical intervention on the carotid blood vessel and the consequent restenosis.
What are the symptoms for narrowing of the carotid arteries?
Minor carotid artery stenoses generally show no symptoms, so sometimes the first sign of carotid artery disease may be a stroke. Temporary ischemic attack (also called TIA or “mini stroke”) is one of the most important warning signs of stroke. TIA occurs when a blood clot briefly blocks an artery that supplies blood to the brain. The following symptoms of TIA, which are temporary and can last for minutes or hours, can occur alone or in combination:
- Sudden loss of vision or blurred vision in one or both eyes
- Weakness and / or numbness on one side of the face, or on one arm or leg, or on one side of the body
- Fuzzy speech, difficulty speaking or understanding what others are saying
- Loss of coordination
- Dizziness or confusion
- Difficulty with swallowing
The TIA requires urgent medical help, because it is impossible to predict whether it will turn into a major stroke. If you or someone you know experiences these symptoms, seek emergency help. Immediate treatment can save your life or increase your chances of complete recovery.
TIAs are strong predictors of future strokes; a person who has experienced a TIA is 10 times more likely to experience a stroke than one who has not experienced a TIA.
What is a stroke?
A stroke occurs when a blood vessel in the brain becomes blocked or ruptured. The brain cannot store oxygen, so it relies on a network of blood vessels to provide it with oxygen-rich blood. Stroke results in a lack of blood supply, due to which the surrounding nerve cells will be cut off from the supply of nutrients and oxygen. When the tissue is cut off from oxygen for more than 3 to 4 minutes, it begins to die.
A stroke can occur if:
- the artery becomes extremely narrowed by plaque
- a piece of plaque breaks off and travels to the smaller arteries of the brain
- a blood clot forms and blocks a narrowed artery
Stroke can also occur as a result of other conditions, such as sudden bleeding in the brain (intracerebral hemorrhage), sudden bleeding in the spinal fluid (subarachnoid hemorrhage), atrial fibrillation, cardiomyopathy or blockage of tiny arteries in the brain.
Diagnostic of carotid disease
If you are at risk for carotid artery disease, it is important that you have regular checkups.
The doctor will examine the arteries in your neck with a stethoscope. An abnormal rush sound, called bruit, may indicate carotid artery disease. However, bruises are not always present when there are blockages and can be heard even when the blockages are less.
Diagnostic tests to assess carotid disease include:
- Carotid artery color Doppler: A recording procedure that uses high-frequency sound waves to examine the carotid arteries to determine if there is a narrowing. This is the most common test used to assess the presence of carotid artery disease.
- Carotid angiography (carotid angiogram): During this invasive imaging procedure, a catheter (a thin, flexible tube) is inserted into a blood vessel in the arm or leg and leads to the carotid arteries with the help of a special X-ray machine. Contrast material is injected through the catheter, while X-rays of the carotid arteries are taken. This test can be performed to assess or confirm the presence of narrowing or blockage in the carotid arteries, determine the risk of future stroke, and assess the need for future treatment, such as carotid stenting or surgery.
- Computed tomography (CT scan): A CT scan of the brain can be performed if a stroke or TIA is suspected to have occurred. During a CT scan, X-rays pass through the body and are captured by detectors in the scanner that produce three-dimensional (3D) images on a computer screen. Depending on the type of scan you need, contrast material can be injected intravenously (into a vein), so that the radiologist can see the body structures on the CT image. This test can detect areas of brain damage.
- CT angiogram (CTA): CT angiography – CTA is a test that uses advanced CT technology, along with intravenous (IV) contrast material (color), to obtain 3D images of high-resolution carotid arteries. CTA scans allow doctors to determine the degree of stenosis in the carotid and spinal arteries, and can also assess the leads to these arteries as well as blood vessels in the brain.
- Magnetic resonance angiogram (MRA): MRA is a type of magnetic resonance imaging (MRI) that uses a magnetic field and radio waves to provide images of the carotid arteries. This test can provide important information about the carotid and vertebral arteries and the degree of stenosis.
Treatment of carotid artery at the PULSE CARDIOLOGY CENTER
How is carotid artery disease treated?
Carotid disease is treated:
- By making lifestyle changes
- Taking prescribed medications
- Intervention – endovascular or surgical procedure
To prevent the progression of carotid artery disease, lifestyle changes are recommended:
- Stop smoking and using tobacco products.
- Control high blood pressure, cholesterol, diabetes and heart disease.
- Go to your doctor for regular check-ups.
- Have your doctor check your lipid status and keep it at normal levels
- Eat food low in saturated fat, cholesterol and sodium.
- Achieve and maintain the desired weight.
- Exercise regularly – at least 30 minutes of exercise most days of the week.
- Limit the amount of alcohol you drink. Alcohol abuse is defined as drinking more than three drinks a day.
Carotid treatments and procedures
There are several options for carotid artery therapy:
- conservative neurological therapy
- surgical intervention
- endovascular, minimally invasive method, which is performed through the artery of the inguinal region using a catheter through which a balloon dilatation is performed and a stent is placed
If there is severe narrowing or blockage of the carotid artery, a procedure may be needed to open the artery and increase blood flow to the brain to prevent future stroke. If you have symptoms associated with carotid artery narrowing, you will probably need to undergo carotid endarterectomy or carotid stenting to correct the narrowing of the artery and reduce the risk of stroke.
If you have asymptomatic carotid stenosis, the specialist will assess the test results and risk status to make a recommendation as to whether medical therapy would be the best option.
Carotid artery surgery
Carotid surgery – carotid endarterectomy is a traditional surgical treatment of carotid artery disease. Carotid endarterectomy has been shown to be useful for symptomatic patients with 50 or more percent of carotid stenosis (blockade) and for asymptomatic patients with 60 or more percent of carotid stenosis.
Carotid endarterectomy can be performed under general anesthesia (the patient is asleep) or local anesthesia with intravenous sedation. During the procedure, an incision is made in the neck at the site of the carotid artery blockage. The surgeon removes the plaque from the artery and when the plaque removal is complete, the surgeon sutures the vessel. Blood flow to the brain is restored in the normal way.
Endovascular treatment of carotid arteries
Endovascular intervention for the treatment of carotid arteries is minimally invasive – non-surgical intervention. Endovascular therapy for internal carotid artery stenosis began with percutaneous balloon angioplasty in the late 1970s in patients deemed unsuitable for carotid endarterectomy. Better stent design allows extensive use of distal embolic protection.
The procedure of carotid angioplasty and stenting is performed while the patient is awake, with the help of sedatives. During the procedure, a balloon catheter is inserted through the sheath into the blood vessel. With X-ray guidance, the catheter is placed through a blood vessel and directed toward the carotid artery at the site of blockage or narrowing. A specially designed guide with filter is placed outside the area of blockage or narrowing.
Once in place, the tip of the balloon is inflated for a few seconds to open or dilate the artery. A filter (called an embolic protective device) collects debris that can break off the blockage. The stent (small mesh tube) is placed in the artery and opens to fit the size of the artery. The stent remains permanently in place and acts as a scaffold to support the artery walls and keep the artery open. After a few weeks, the artery heals around the stent.
Carotid surgery or a minimally invasive method to treat carotid disease?
Research has shown that carotid stenting, when used with an embolism protection device, is as safe and effective as carotid endarterectomy in high-risk surgical patients. Recovery from both carotid endarterectomy and carotid angioplasty and stenting usually requires a hospital stay of one night. Endovascular treatment of carotid arteries does not require general anesthesia, there are no cuts on the neck and recovery is easier. Patients often return to regular activities within one to two weeks after these procedures.
Risk factors for carotid artery disease
Risk factors associated with the development of atherosclerosis include:
- Family history of atherosclerosis (either carotid artery disease or coronary artery disease or elsewhere in the vascular system)
- Age: In general, the risk of atherosclerosis increases as we age, and especially men younger than 75 have a higher risk of developing carotid artery disease than women, but after age 75 women have a higher risk than men
- Hyperlipedemia – high levels of fat (LDL, bad cholesterol) and triglycerides in the blood. However, this connection is not as strong as in coronary artery disease
- Smoking
- High blood pressure (hypertension)
- Diabetes
- Obesity
- Physical inactivity
Typically, carotid arteries become diseased a few years later than coronary arteries. People who have coronary artery disease and atherosclerosis elsewhere (such as peripheral artery disease) have a higher risk of developing carotid artery disease.
