Home » Services » Interventional procedures » Myoma embolization
Myoma embolization
Benign tumors of the uterus can be leiomyomas, fibroids, fibromyomas.
Uterine fibroids -myoma are benign tumors of the uterus, the origin of smooth muscles. Myoma often cause abnormal vaginal bleeding (eg, menorrhagia, menometrorrhagia), pelvic pain and pressure, urinary and digestive problems, and pregnancy complications. The diagnosis is made by gynecological examination and other tests. Treatment of patients with symptoms depends on their desire to preserve fertility and the uterus and may include oral contraceptives, short-term preoperative use of gonadotropin-releasing hormone to reduce fibroids, and final surgical solutions (eg myomectomy, hysterectomy), endometrial ablation.
Types of myoma
Uterine myoma are the most common tumors in the pelvis, and they occur in 70% of women. However, many fibroids are small and asymptomatic. The risk of fibroids includes women with colored skin and those with a high body mass index. Possible factors are giving birth and smoking cigarettes.
Most uterine fibroids are submucosal, followed by intramural and then subserous. Sometimes fibroids appear primarily in the broad ligament (intraligamentary), fallopian tubes or cervix. Some fibroids have a stalk. Fibroids are usually multiple but all develop from a single monoclonal smooth muscle cell. Because they have estrogen receptors, fibroids often increase during the reproductive years and decrease after menopause.
Degeneration begins with loss of blood supply and is described as hyaline, myxomatous, calcifying, cystic, fatty, red (usually only during pregnancy) or necrosis. Although patients are often concerned about myoma, sarcomatous changes are very rare.
Symptoms and signs of fibroids
Myoma can cause menorrhagia or menometrorrhagia. If the fibroids grow and degenerate or bleed inside them, or if the fibroids on the petiole turn around the petiole, severe acute or chronic pressure or pain may follow. Urological symptoms (eg need to urinate frequently) may be due to pressure on the bladder and digestive symptoms (eg constipation) may be due to pressure on the bowel. Fibroids can prevent pregnancy; during pregnancy they can cause recurrent miscarriages, premature births or abnormal positions and make a caesarean section necessary.
If you’ve been diagnosed with having uterine fibroids, there are many treatment options for you to consider. Fibroids are the most frequently seen tumors of the female reproductive system and more than 99 percent of the time the tumors are benign (non-cancerous).
Though most are benign, they may range in size, from the size of a pea to the size of a softball or small grapefruit and can cause heavy periods, pelvic pressure, bloating, urinary frequency, and constipation. Treatments can vary from monitoring to a hysterectomy and will vary depending on the patient’s age, symptoms, previous treatments and successes, and desire to have children.
Nine out of 10 patients who undergo uterine fibroid embolization will experience significant improvement or their symptoms will go away completely with minimal recovery time.
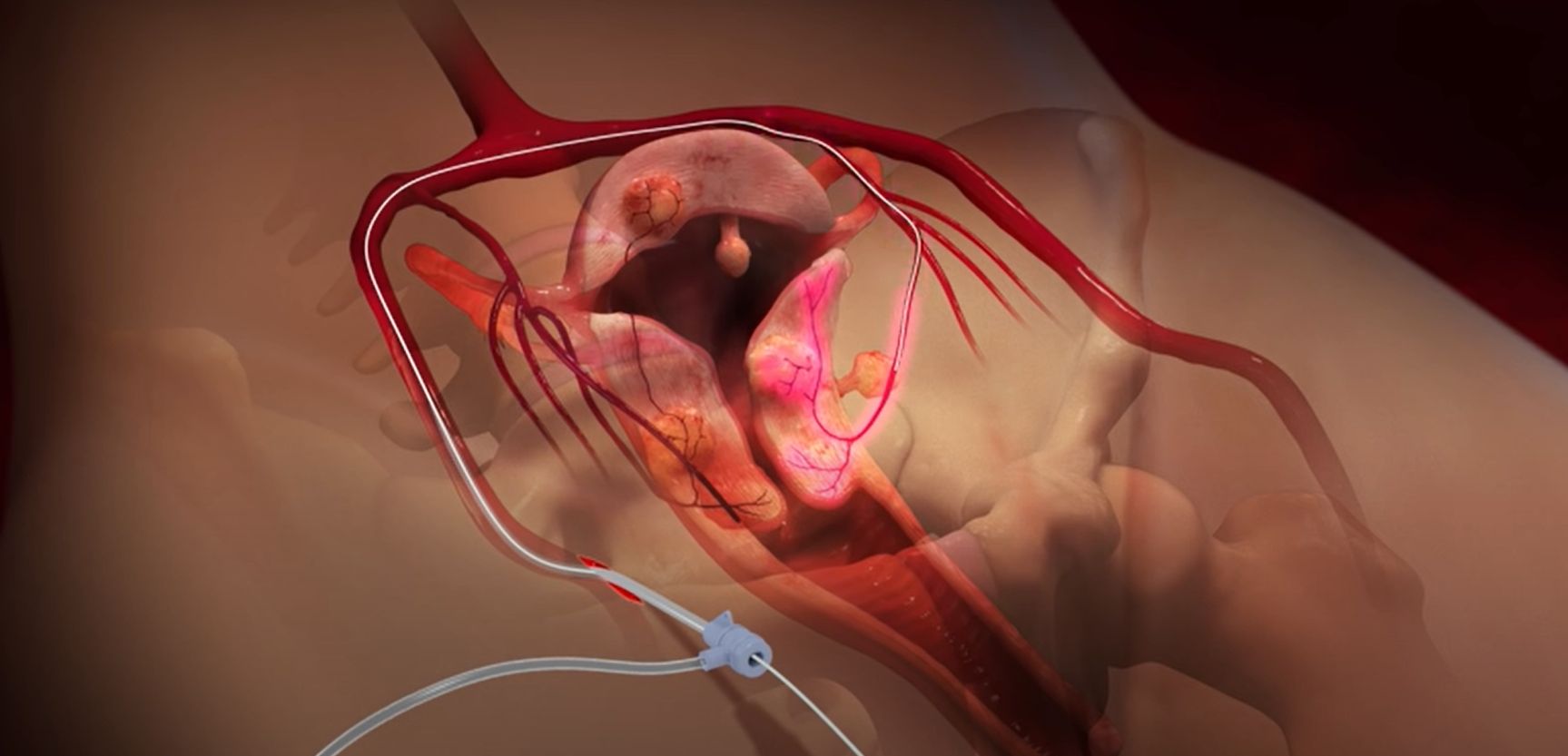
Uterine myoma embolization is a minimally invasive procedure used to treat fibroid tumors of the uterus which can cause heavy menstrual bleeding, pain, and pressure on the bladder or bowel. It uses a form of real-time x-ray called fluoroscopy to guide the delivery of embolic agents to the uterus and fibroids. These agents block the arteries that provide blood to the fibroids and cause them to shrink. Studies have shown that nearly 90 percent of women who undergo UFE experience significant or complete resolution of their fibroid-related symptoms.
What is Uterine Myoma Embolization
Uterine fibroid embolization (UFE) is a minimally invasive treatment for fibroid tumors of the uterus. The procedure is also sometimes referred to as Uterine Artery Embolization (UAE), but this term is less specific and, as will be discussed below, UAE is used for conditions other than fibroids.
Fibroid tumors, also known as myomas, are benign tumors that arise from the muscular wall of the uterus. It is extremely rare for them to turn cancerous. More commonly, they cause heavy menstrual bleeding, pain in the pelvic region, and pressure on the bladder or bowel.
In a UFE procedure, physicians use an x-ray camera called a fluoroscope to guide the delivery of small particles to the uterus and fibroids. The small particles are injected through a thin, flexible tube called a catheter. These block the arteries that provide blood flow, causing the fibroids to shrink. Nearly 90 percent of women with fibroids experience relief of their symptoms.
Because the effect of uterine fibroid embolization on fertility is not fully understood, UFE is typically offered to women who no longer wish to become pregnant or who want or need to avoid having a hysterectomy, which is the operation to remove the uterus.
What are some common uses of the embolization procedure?
Uterine artery embolization has been used for decades to stop severe pelvic bleeding caused by:
- trauma
- malignant gynecological tumors
- hemorrhage after childbirth
Things You Should Know About Uterine Fibroid Embolization
- It’s a non-surgical, minimally invasive treatment option for uterine fibroids
- Your uterus remains preserved
- Lower complication rate with reductions in pain and blood loss
- Reduced recovery time so most patients return home the same day and return to normal activities within one week
How is the procedure performed?
Myoma embolization is an image-guided, minimally invasive procedure that uses a high-definition x-ray camera to guide a trained specialist, most commonly an interventional radiologist to introduce a catheter into the uterine arteries to deliver the particles. The procedure is typically performed in a Cath-lab or occasionally in the operating room.
You will lie on the procedure table.
The doctor or nurse may connect you to monitors that track your heart rate, blood pressure, oxygen level, and pulse.
A nurse or technologist will insert an intravenous (IV) line into a vein in your hand or arm to administer a sedative. This procedure may use moderate sedation. It does not require a breathing tube. However, some patients may require general anesthesia.
The nurse will sterilize the area of your body where the catheter is to be inserted. They will sterilize and cover this area with a surgical drape.
Your doctor will numb the area with a local anesthetic. This may briefly burn or sting before the area becomes numb.
The doctor will make a very small skin incision at the site.
Using x-ray guidance, a catheter is inserted into your femoral artery, which is located in the groin area. A contrast material provides a roadmap for the catheter as it is maneuvered into your uterine arteries. The embolic agent is released into both the right and left uterine arteries by repositioning the same catheter that was originally inserted. Only one small skin puncture is required for the entire procedure.
When the procedure is complete, the doctor will remove the catheter and apply pressure to stop any bleeding. Sometimes, your doctor may use a closure device to seal the small hole in the artery. This will allow you to move around more quickly. No stitches are visible on the skin. The nurse will cover this tiny opening in the skin with a dressing.
The doctor or nurse will remove your IV line before you go home.
You will most likely remain in the hospital overnight so that you may receive pain medications and be observed.
This procedure is usually completed within 90 minutes.
What would make me ineligible for UFE?
Patients should discuss their ability to proceed with UFE with their provider. Patients with an active pelvic infection, certain uncorrectable bleeding problems, endometrial cancer, extremely large fibroids, or a desire for fertility preservation are poor candidates for this procedure.
What happens after myoma embolization
Most patients go home the same or the next day with cramps and pain. Fever is an occasional side effect that is treated with medication. Many women resume light activity within a few days and regular activity within a week. Embolization is effective in multiple fibroids, and recurrence of treated fibroids is very rare.
Monitoring is done one month after the intervention, and magnetic resonance imaging is done after six months to check for improvement in symptoms and again in a year if symptoms persist.
How should I prepare for myoma embolization
Imaging of the uterus by magnetic resonance imaging (MRI) or ultrasound is performed prior to the procedure to determine if fibroid tumors are the cause of your symptoms and to fully assess the size, number and location of the fibroids.
Occasionally, your gynecologist may want to take a direct look at the uterus by performing a laparoscopy. If you are bleeding heavily in between periods, a biopsy of the endometrium (the inner lining of the uterus) may be performed to rule out cancer
Tell your doctor about all the medications you take, including herbal supplements. List any allergies, especially to local anesthetic, general anesthesia, or contrast materials. Your doctor may tell you to stop taking aspirin, nonsteroidal anti-inflammatory drugs (NSAIDs) or blood thinners before your procedure.
Tell your doctor about recent illnesses or other medical conditions.
Women should always tell their doctor and technologist if they are pregnant. Doctors will not perform many tests during pregnancy to avoid exposing the fetus to radiation. If an x-ray is necessary, the doctor will take precautions to minimize radiation exposure to the baby. Your doctor will likely tell you not to eat or drink anything after midnight before your procedure.
Your doctor will tell you which medications you may take in the morning.
You should plan to stay overnight at the hospital following your procedure.
The nurse will give you a gown to wear during the procedure.
Myoma embolization benefits vs. risks
Benefits
Uterine fibroid embolization, done under local anesthesia, is much less invasive than open or laparoscopic surgery to remove individual uterine fibroids (myomectomy) or the whole uterus (hysterectomy).
No surgical incision is necessary—only a small nick in the skin that does not need stitches.
Patients ordinarily can resume their usual activities much earlier than if they had surgery to treat their fibroids.
As compared to surgery, general anesthesia is not required and the recovery time is much shorter, with virtually no blood loss.
Follow-up studies have shown that nearly 90 percent of women who have their fibroids treated by uterine fibroid embolization experience either significant or complete resolution of their fibroid-related symptoms. This is true both for women who have heavy bleeding as well as those who have bulk-related symptoms including urinary frequency, pelvic pain or pressure. On average, fibroids will shrink to half their original volume, which amounts to about a 20 percent reduction in their diameter. More importantly, they soften after embolization and no longer exert pressure on the adjacent pelvic organs.
Follow-up studies over several years have shown that it is rare for treated fibroids to regrow or for new fibroids to develop after uterine fibroid embolization. This is because all fibroids present in the uterus, even early-stage nodules that may be too small to see on imaging exams, are treated during the procedure. Uterine fibroid embolization is a more permanent solution than the option of hormonal therapy, because when hormonal treatment is stopped the fibroid tumors usually grow back. Regrowth also has been a problem with laser treatment of uterine fibroids.
Risks
Any procedure that places a catheter inside a blood vessel carries certain risks. These risks include damage to the blood vessel, bruising or bleeding at the puncture site, and infection. The doctor will take precautions to mitigate these risks.
When performed by an experienced interventional radiologist, the chance of any of these events occurring during uterine fibroid embolization is less than one percent.
Any procedure that penetrates the skin carries a risk of infection. The chance of infection requiring antibiotic treatment appears to be less than one in 1,000.
There is always a chance that an embolic agent can lodge in the wrong place and deprive normal tissue of its oxygen supply.
An occasional patient may have an allergic reaction to the x-ray contrast material used during uterine fibroid embolization. These episodes range from mild itching to severe reactions that can affect a woman’s breathing or blood pressure. Women undergoing UFE are carefully monitored by a physician and a nurse during the procedure, so that any allergic reaction can be detected immediately and addressed.
Approximately two to three percent of women will pass small pieces of fibroid tissue after uterine fibroid embolization. This occurs when fibroids located inside the uterine cavity detach after embolization. Women with this problem may require a procedure called D & C (dilatation and curettage) to be certain that all the material is removed to prevent bleeding or infection from developing.
In the majority of women who undergo uterine fibroid embolization, normal menstrual cycles resume after the procedure. However, in approximately one percent to five percent of women, menopause occurs after uterine fibroid embolization. This appears to occur more commonly in women who are older than 45 years.
Although the goal of uterine fibroid embolization is to cure fibroid-related symptoms without surgery, some women may eventually need to have a hysterectomy because of infection or persistent symptoms. The likelihood of requiring hysterectomy after uterine fibroid embolization depends on how much time elapses until menopause. The younger the patient, the greater the tendency to develop new fibroids or recurrent symptoms.
Women are exposed to x-rays during uterine fibroid embolization, but exposure levels usually are well below those where adverse effects on the patient or future childbearing would be a concern.
The question of whether uterine fibroid embolization impacts fertility has not yet been answered, although a number of healthy pregnancies have been documented in women who have had the procedure. Physicians may recommend that a woman who wishes to have more children consider surgical removal of the individual tumors rather than undergo uterine fibroid embolization. If this is not possible, then UFE may still be the best option. It is not possible to predict whether the uterine wall is in any way weakened by UFE, which might pose a problem during delivery. Therefore, the current recommendation is to use contraception for six months after the procedure and to undergo a Cesarean section during delivery rather than to risk rupture of the wall of the uterus from the intense muscular contractions that occur during labor.
