Home » Services » Interventional procedures » Biliary stent placement
Biliary stent placement
A biliary stent, also known as a bile duct stent, is a thin, hollow tube that is placed in the bile duct. The stent holds the duct open after the duct has been blocked or partly blocked.
Fluids like bile need to flow through your bile duct into your intestine to help digestion. If the duct is blocked, these fluids can build up in the liver. This can cause symptoms such as jaundice (yellowing of your skin and whites of your eyes), belly pain, and nausea. Bile that isn’t draining as it should, can get infected.
Opening up the duct with a stent allows bile to drain and can help you feel better.
There are two ways your doctor can place a bile duct stent: ERCP and PTC.
ERCP (endoscopic retrograde cholangiopancreatography)
In an ERCP, the doctor will use a tool called an endoscope, or scope. It is a thin, lighted tube that bends. It has a camera on it so the doctor can guide the scope to the bile duct. The doctor uses the scope to put a metal or plastic tube in the bile duct. This can help open the duct.
Before the test, you may get medicine to numb the back of your throat. You also will get medicine to help you relax. During the test, you may be asked to lie on your side.
PTC (percutaneous transhepatic cholangiography)
In a PTC, the doctor moves a long needle through your belly and into the liver. The needle is used to inject dye into the liver. X-rays are taken while the dye moves through the bile ducts. The doctor will take that needle out and insert a special hollow tube into the bile duct. The doctor will then move the stent through this tube and place it in the bile duct.
You will get medicine to numb your skin and keep you comfortable during the test. Some patients will require a general anesthetic.
What is biliary stenting?
Sometimes the biliary drainage procedure may be extended with the placement of a permanent plastic or metal stent across the site of the bile duct blockage. Stents are usually inserted a few days after the initial drainage procedure and they keep the narrowed duct open without the need for a catheter.
Stenting may be preceded or followed by biliary dilatation, which involves dilating a segment of bile duct with a balloon to open up the stricture.
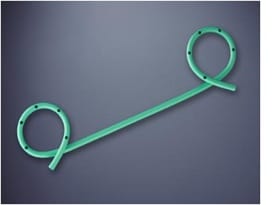
A plastic biliary stent
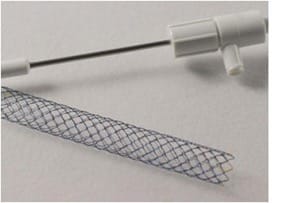
A metal biliary stent
What are the indications for percutaneous biliary drainage +/- stenting?
The most common indication for biliary drainage is blockage or narrowing (stricture) of the bile ducts. There are several conditions that may cause this including:
- Gallstones – in the gallbladder or within the bile ducts
- Inflammation of the pancreas (pancreatitis)
- Inflammation of the bile ducts (sclerosing cholangitis)
- Tumours of the pancreas, gallbladder, bile duct, liver
- Enlarged lymph nodes in the region of the pancreas and liver due to various types of tumours
- Injury to bile ducts during surgery
- Infection
Biliary drainage relieves obstruction by providing an alternative pathway to exit the liver.
Biliary drainage may also be necessary if a hole develops in the bile duct, resulting in leakage of bile into the abdominal cavity. This leak may cause severe pain and infection. Biliary drainage stops the leak and helps the hole in the bile duct to heal.
Biliary drainage may be necessary in preparation for surgery or other procedure on the bile ducts, such as removal of a bile duct stone or tumour.
Follow-up care is a key part of your treatment and safety.
Be sure to make and go to all appointments and call your doctor or nurse call line if you are having problems. It’s also a good idea to know your test results and keep a list of the medicines you take.
How do you prepare for the procedure?
Do not eat or drink for 6 to 8 hours before the procedure.
Be sure you have someone to take you home. Some medicines you’ll get during the procedure will make it unsafe for you to drive or get home on your own.
Understand exactly what procedure is planned, along with the risks, benefits, and other options.
Tell your doctor ALL the medicines and natural health products you take. Some may increase the risk of problems during the procedure. Your doctor will tell you if you should stop taking any of them before the procedure and how soon to do it.
If you take aspirin or some other blood thinner, be sure to talk to your doctor. They will tell you if you should stop taking it before your procedure. Make sure that you understand exactly what your doctor wants you to do.
Tell your doctor if you have an allergy to contrast (dye used for some X-rays).
Make sure your doctor and the hospital have a copy of your advance care plan. If you don’t have one, you may want to prepare one. It lets others know your health care wishes. It’s a good thing to have before any type of surgery or procedure.
You may be asked to have bloodwork done before your procedure.
What happens on the day of the procedure?
- Follow the instructions exactly about when to stop eating and drinking. If you don’t, your procedure may be cancelled. If your doctor told you to take your medicines on the day of the procedure, take them with only a sip of water.
- Take a bath or shower before you come in for your procedure. Do not apply lotions, perfumes, deodorants, or nail polish.
- Take off all jewellery and piercings. Take out contact lenses if you wear them.
At the hospital
Bring your ID card and medical history with you.
You may get medicine that relaxes you or puts you in a light sleep. The area being worked on will be numb. Children may have general anesthetic – special medicine to make them sleep more deeply.
For an ERCP, the doctor may send puffs of air through the tube to see better. This may make you feel bloated.
You may feel some bloating or cramping as the ERCP tube is moved. If you are very uncomfortable, you can let the doctor know with a signal or a tap on the arm. You and your doctor can agree on this signal before the test.
After an ERCP, you will stay at the hospital or clinic for 1 to 2 hours until the numbing medicine and medicines that helped you relax or sleep wears off.
After a PTC, you will be on bedrest for several hours. Your healthcare team will monitor you closely for bleeding or other problems. Your doctor will assess you and talk to you about when you can go home.
When should you call your doctor?
- You have questions or concerns.
- You don’t understand how to prepare for your procedure.
- You become ill before the procedure (such as fever, flu, or a cold).
- You need to reschedule or have changed your mind about having the procedure.
