call us
Endovascular treatment for abdominal aorta
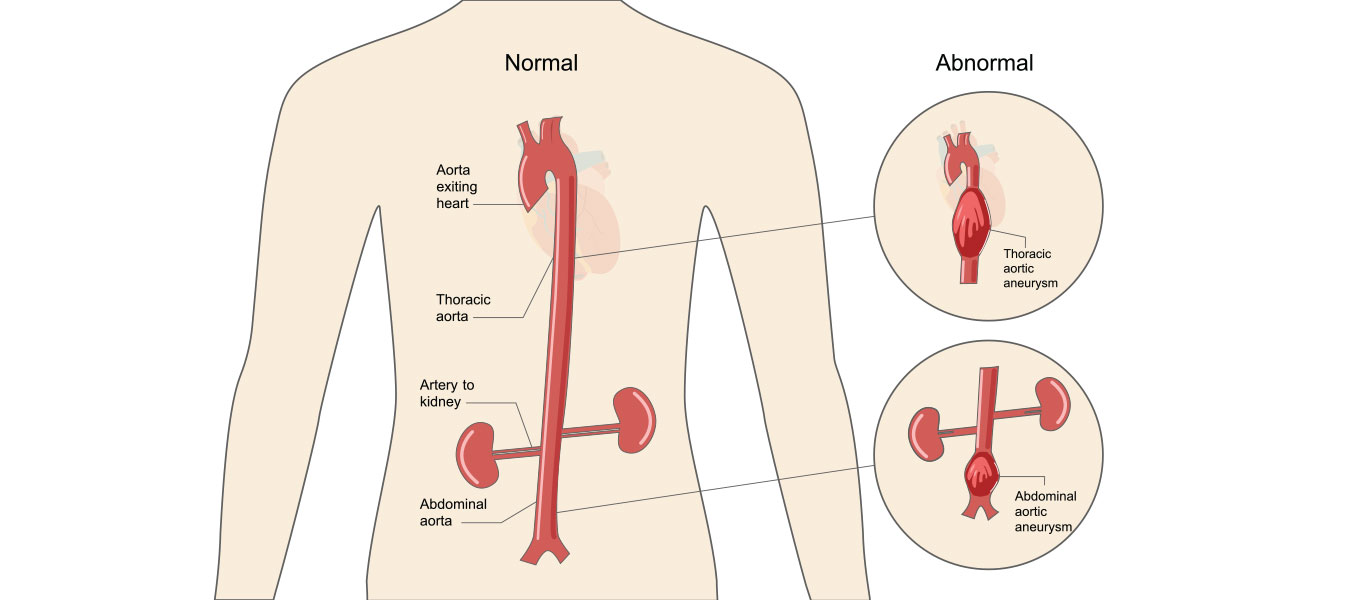
The abdominal aorta is the main blood vessel in the abdominal cavity that continues to the thoracic aorta, which is the main blood vessel in the chest, and which eventually divides into two blood vessels (iliac arteries) that go to both lower extremities. The abdominal aorta is prone to dilate in its final part when from a normal diameter (up to 2cm) it can expand to over 6cm. This enlargement of the aorta in the abdomen is called an abdominal aortic aneurysm.
Men over the age of 65 are at particular risk for developing abdominal aortic aneurysms. Did you know that rupture of the abdominal aortic aneurysm brings great mortality and that the only cure is emergency surgery. This is the reason why preventive examinations are recommended for men older than 65.
How does an abdominal aortic aneurysm form?
It is a gradual process that sometimes takes decades. Gradual weakening of the aortic wall leads to its relaxation and thus expansion. Weakening of the aortic wall is encouraged by the gradual “aging” of the blood vessel wall, which is a consequence of long-term blood flow, the formation of atherosclerotic deposits and increased pressure. These processes are accelerated by the influence of tobacco products (nicotine), while in some people this process is accelerated if there is a genetic predisposition associated with congenital weakening of the aortic wall. Once the process begins it gradually progresses and the aneurysm gradually grows.
What size should an abdominal aneurysm be in order to have surgery
An aortic aneurysm gradually grows until the moment when it ruptures, which is often fatal. The process of aneurysm growth is accelerated in smokers, people with high blood pressure (especially if it is not under control) and lung diseases. This growth is 1-3 mm per year, but in certain periods this growth can be accelerated. By correcting the risk factors and quitting smoking, this process of aneurysm growth can be slowed down and even stopped. The faster the aneurysm grows, the bigger the aneurysm, and thus the risk of bursting increases with increasing diameter. A limit of 55mm for men and 50mm for women has been set as the limit beyond which the risk of cracking increases significantly.
What is endovascular treatment of abdominal aortic aneurysm
The aorta is the largest blood vessel in the body and carries blood from the heart to the rest of the organs. An aneurysm occurs if the arterial wall weakens and develops a bulge, which means that blood flows to the weakened area. Abdominal aortic aneurysms can weaken the aorta, the largest blood vessel in your body. This can develop into a potentially serious health problem that can be fatal if the aneurysm ruptures, causing massive internal bleeding.
Abdominal aortic aneurysms (AAAs) are also known as “silent killers” because when they enlarge and rupture, there is an 80-90% risk of imminent death.
Endovascular treatment of the abdominal aorta is a minimally invasive procedure in which an interventional radiologist places a covered stent (a metal mesh tube covered with tissue) in the area with the aneurysm so that blood can flow through the blood vessel. A stent is inserted through a catheter through an artery in the patient’s groin, using X-rays to guide the stent to the aneurysm.
When to perform an intervention on the abdominal aorta
If you have a small abdominal aortic aneurysm less than 5 cm in diameter, it is unlikely to rupture, so it is recommended that the vascular surgeon regularly monitor and control the aneurysm. However, if you have an aneurysm smaller than 5 cm, but it grows by more than 1 cm each year or causes symptoms such as back pain and tenderness, endovascular treatment of the abdominal aorta is the right choice for you.
If your aneurysm is larger than 5 cm, you will need treatment to prevent the aneurysm from rupturing.
Endovascular treatment of the abdominal aorta at the Pulse Cardiology Center
Endovascular stent graft or endovascular aneurysm treatment is a newer form of treatment for abdominal aortic aneurysm that is less invasive than open surgery – classic abdominal aneurysm surgery. Endovascular treatment of the abdominal aorta uses an endovascular stent graft to strengthen the aortic wall and help prevent the damaged area from rupturing.
The word endovascular refers to an area inside a blood vessel such as the aorta. With endovascular stent graft therapy, an endovascular stent graft is placed inside the abdominal aorta to protect the aneurysm from rupture.
The stent graft is placed inside the aortic aneurysm using a long, very thin, soft, plastic tube called a delivery catheter. The delivery catheter contains a compressed stent graft.
Minimally invasive treatment for abdominal aortic aneurysms
You will receive a combination of epidural and local anesthesia for the procedure. An interventional radiologist will make a small incision at the top of each leg so that he can insert a short tube (known as a sheath) that allows safe access to the blood vessels in the groin. Using guiding fluoroscopy, the interventional radiologist will insert guides and catheters (thin flexible tubes). Contrasting material (color) will be injected into the treated area, so that the exact location of the aneurysm can be seen on the images. The interventional radiologist will then use a guide to move the stent to the aneurysm.
When the stent is placed in the right place, it will expand, sealing the aneurysm and restoring normal blood flow through the blood vessel. An endovascular stent is inserted inside the abdominal aorta to prevent the aneurysm from rupturing.
After the procedure, the Pulse Cardiology Center team will monitor your vital parameters and you will stay in the hospital for 2-3 days. You may experience bruising and pain, although this can be treated with standard painkillers. Movement is encouraged when you get up. You will need to have the stent examined regularly by CT or ultrasound to make sure it is in good condition and to avoid long-term problems.
Abdominal aorta intervention risks
Endovascular treatment of the abdominal aorta is recommended as a preventive treatment to avoid aneurysm rupture and certain death. Most patients do not suffer immediate major problems and aneurysm rupture is avoided in over 99% of patients. The rates of pain and serious complications are lower than with surgery, but the main limitations of endovascular intervention on the abdominal aorta are that the stent can be moved to another area of the body and blood begins to collect again in the aneurysm. This means that you will need regular monitoring. If any problems arise, they can be resolved as soon as possible.
Minor complications include the risk of bruising and infection. There are some serious complications associated with the procedure, including death, stroke, tissue death, limb loss, and kidney injury. It is estimated that the rate of serious complications is less than 15%, and the risk of death during the procedure is less than 1.5%, which is almost three times less than the risk of dying during open surgery (about 4.5%). Some patients react to iodine in a contrasting color used for imaging, which can affect the kidneys.
Endovascular treatment or surgery of the abdominal aneurysm
Endovascular stent graft and open surgery – abdominal aortic surgery, are done to prevent rupture of the abdominal aortic aneurysm. The difference is that an endovascular stent transplant is placed inside the aneurysm without removing tissue from the aorta and does not require open chest or open abdominal surgery.
Because it is less invasive than open surgery, recovery time for endovascular stent grafting may be faster.
Usually, the patient can return home in a week, and return to normal activities in 4 to 6 weeks.
More information about abdominal aneurysm and treatment at the Pulse Cardiology Center
If you need additional information or want to schedule an examination at the Pulse Cardiology Center, you can contact us at: +381117555000 or you can schedule an examination online.
