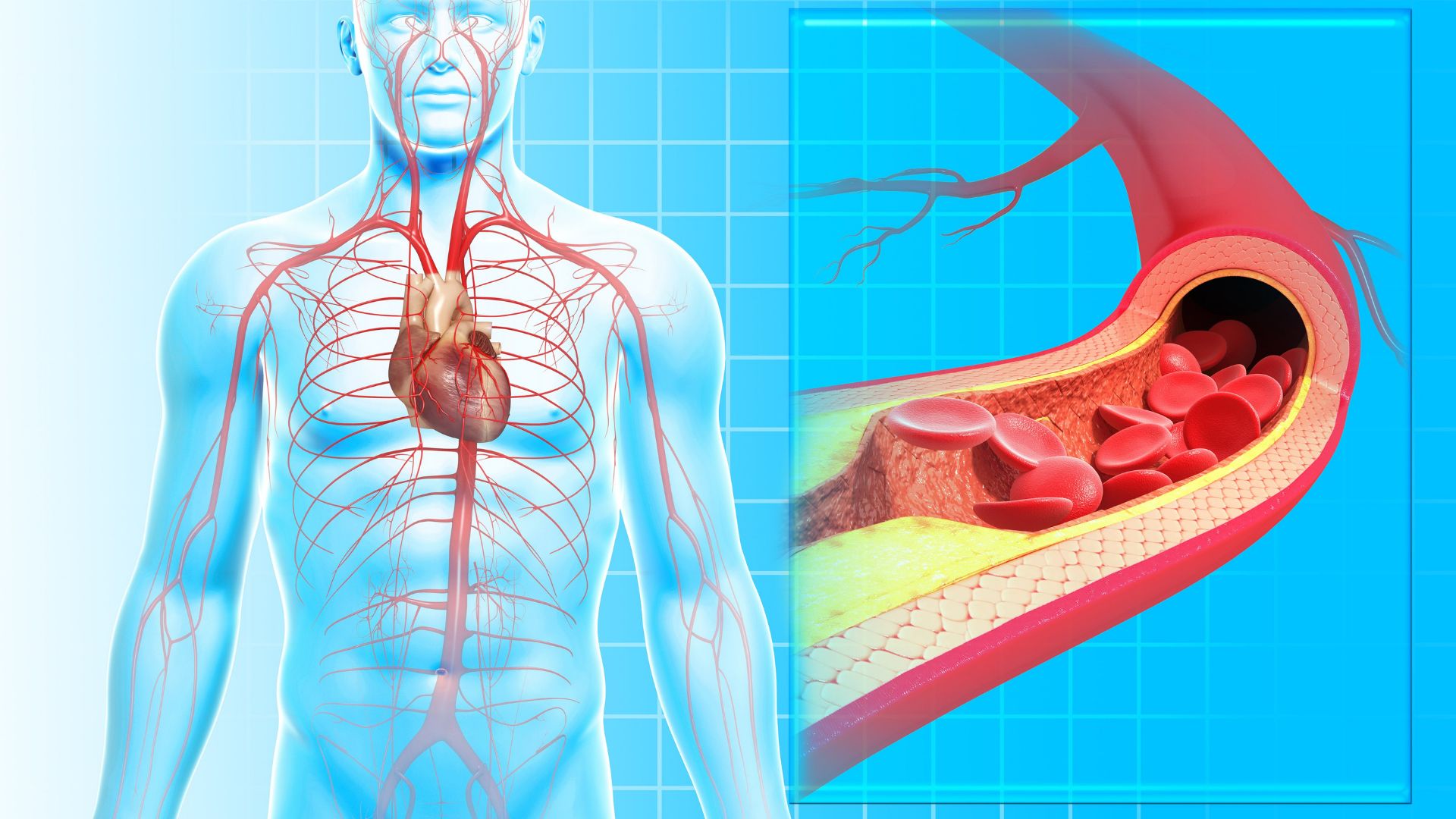
Ischemic heart disease, or coronary artery disease, is the term used for a group of cardiovascular diseases that occur due to reduced blood flow through the arteries that supply blood and oxygen to the heart. In about 95% of cases, atherosclerosis is the “culprit” for the reduced blood flow through the arteries. In the remaining 5% of cases, the cause is some form of coronary vessel anomaly.
Symptoms of ischemic heart disease:
- Chest pain
- Uncomfortable feeling of pressure in the chest
- Pain and stiffness in the extremities, neck, or back
- Shortness of breath, fatigue, and sometimes chest pain during less physical activity
- Weakness
Atherosclerosis as the main cause of ischemic heart disease
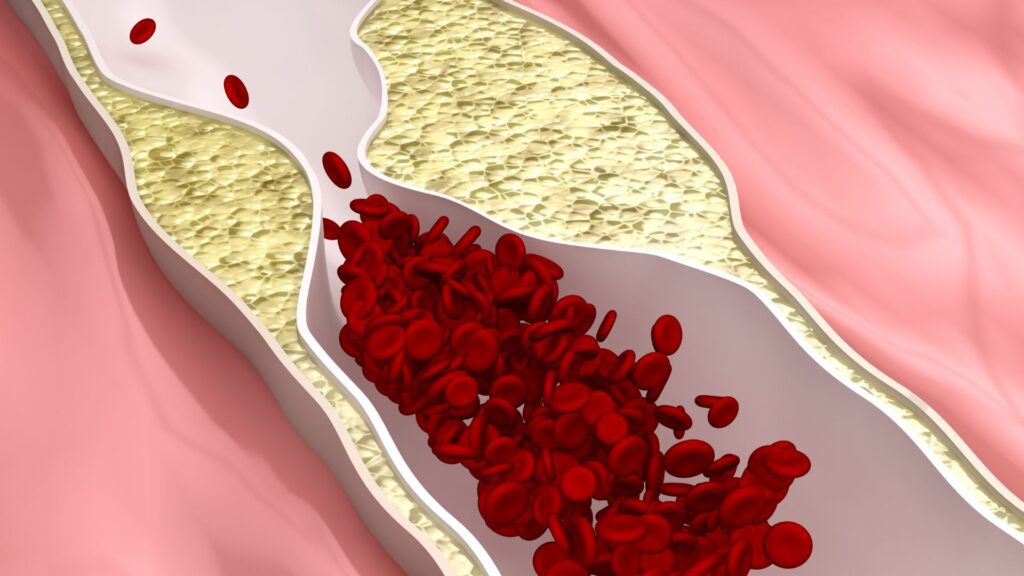
Atherosclerosis as the main cause of ischemic heart disease represents a process of fatty deposit buildup that begins in early adulthood. Over time, there is an accumulation of fat in the walls of blood vessels, leading to narrowing of their lumen and impaired blood flow through them. The risk of coronary artery disease increases with age. Unlike men who are at risk from the age of 40, women’s risk increases after the age of 50, after entering menopause. From the age of 60, both men and women are equally exposed to the risk of ischemic heart disease.
The process of atherosclerosis development is silent and insidious because it does not produce any symptoms, so it is relatively late discovered through non-invasive methods (stress test), when more than two-thirds of the lumen of blood vessels are narrowed due to the deposition of atherosclerotic plaques.
Stable and unstable atherosclerotic plaques
Atheromas (atherosclerotic plaques, fatty deposits on the walls of the heart’s blood vessels) can be either stable or unstable. Stable atheromas have a firm fibrous cap that protects them from damage and rupture. In contrast, unstable atheromas are much more dangerous as they have a thin fibrous cap that is prone to rupture, leading to various complications, including thrombosis.
Complications of atherosclerosis
Blood vessels affected by an atherosclerotic plaque are prone to serious complications such as:
-Calcification: Causes loss of elasticity in the blood vessel.
-Ulceration, fissures, and rupture: Leads to the release of a thrombus that travels to vital organs, causing ischemia (necrosis).
-Hemorrhage: Reduces the lumen of the blood vessel and increases the risk of rupture.
-Aneurysm: Expansion of the blood vessel wall, making it more susceptible to rupture.
Diagnosis of ischemic heart disease
The diagnosis of ischemic heart disease is based on medical history, blood analysis, and physical examination, which may involve one or more diagnostic procedures.
Exercise stress test (ergometry): This procedure assesses the impact of physical exertion on heart function. Ischemic heart disease significantly impairs this ability, worsening the patient’s condition during exertion.
Electrocardiogram (ECG): It monitors the heart’s activity and can indicate rhythm changes, often revealing whether a heart attack has already occurred or is currently happening. If necessary, wearing an ECG Holter monitor may be recommended to assess blood flow disturbances to the heart.
Echocardiography: This method provides various information, including the size and shape of the heart, location and size of cardiac tissue damage, and the appearance of heart valves.
Cardiac catheterization: It is a minimally invasive method to study the heart and the blood vessels that supply it (coronary arteries) without surgical intervention. It typically involves imaging the heart’s arteries (coronary arteries) using X-rays through a technique called coronary angiography. The obtained images are called coronary angiograms or arteriograms.
Cardiac CT (computed tomography): It is a heart scan, also known as coronary calcium scoring, which is a specialized X-ray test that provides images of your heart. These images can help the doctor detect and measure calcium-containing plaques in the arteries.
Forms of Cardiac Ischemia
Cardiac ischemia can manifest through several heart conditions, including:
Angina Pectoris
Angina pectoris is a condition characterized by reduced oxygen supply to the heart muscle. The decreased oxygen supply can be a result of narrowed coronary arteries, but it can also occur when the heart muscle has an increased oxygen demand, as is the case in patients with hyperthyroidism or severe anemia. There are multiple types of this condition, and you can read more about them in our article “Symptoms and Treatment of Angina Pectoris.”
Acute Myocardial Infarction
A heart attack, or acute myocardial infarction, is a serious and urgent medical condition in which the blood supply to the heart is suddenly blocked, usually by a blood clot. The lack of blood in the heart can severely damage the cardiac muscle and can be life-threatening. You can read all about a heart attack in the article “Heart Attack – Myocardial Infarction.”
Arrhythmia
Irregular heart rhythm, whether it is slower or faster than usual, is called arrhythmia. The causes of arrhythmia can vary, but it may also be associated with heart diseases. Everything you need to know about arrhythmia can be found in the article “Skipping Heartbeats – Arrhythmia and Symptoms.”
Heart Failure (Insufficiency)
Heart failure, or cardiac insufficiency, refers to the presence of problems with the heart muscle’s ability to pump blood through the body as it should. As a result, an insufficient amount of oxygen reaches certain parts of the body, while the body is unable to eliminate metabolic byproducts, leading to fluid retention in certain areas, particularly the lungs. This is one of the very dangerous and potentially fatal heart problems, often detected in later stages when treatment is challenging and usually lifelong. Learn more about heart failure in the article “Heart Failure – Insufficiency.”
Sudden Cardiac Death
One of the common causes of death among adults is sudden cardiac death (SCD) resulting from heart diseases. Coronary heart disease accounts for 80-85% of all SCD cases.
Ischemic heart disease accounts for 15.9% of deaths in Serbia
Cardiovascular diseases, with a contribution of 47.3% to all causes of death, are the leading cause of mortality in Serbia. Cardiovascular diseases include rheumatic heart disease accounting for 0.9% of all cardiovascular disease-related deaths, hypertensive heart disease accounting for 16.8%, ischemic heart diseases accounting for 15.9%, cerebrovascular diseases accounting for 17.8%, and other heart and circulatory system diseases accounting for 42.5% of all cardiovascular disease-related deaths.
As the most severe form of ischemic heart disease, acute coronary syndrome is a leading health problem in developed countries worldwide and in developing countries in recent decades.
Acute coronary syndrome includes acute myocardial infarction, unstable angina, and sudden cardiac death.
In Serbia, acute coronary syndrome accounted for 49.9% of all deaths from ischemic heart disease in 2020.
(Data from the Institute of Public Health “Dr Milan Jovanović Batut”)
HEAD 2 Risk factors for cardiac ischemia
Unhealthy lifestyle (smoking, obesity, physical inactivity, alcohol consumption)
Family history of ischemic heart disease
Hypertension
Elevated LDL cholesterol levels and low HDL cholesterol levels
High triglyceride levels
Diabetes
Men over the age of 40
Postmenopausal women
Sleep apnea
Cardiac Ischemia – Natural Treatment
Research shows that adopting healthier lifestyle habits reduces the risk of developing ischemic heart disease.
The first step is to completely give up unhealthy habits such as smoking and excessive alcohol consumption.
Introduce a healthy diet rich in fiber, with lower levels of fat, sugar, and salt.
Engage in regular physical activity, best determined in consultation with a doctor.
If you already have any vascular changes, elevated cholesterol or triglyceride levels, your doctor will prescribe medication therapy.