Everything you need to know about restenosis, the re-narrowing of blood vessels: symptoms, causes, and treatment.
Restenosis is a condition that occurs when an artery, which has been expanded through the placement of a stent or angioplasty, narrows again. Stents are often inserted to treat artery narrowing caused by atherosclerosis, allowing blood to flow freely to the heart. When this area narrows again, restenosis occurs. This condition typically occurs three to six months after stent placement, and very rarely after one year or more.
Statistics show that 3% to 20% of people with drug-eluting stents develop restenosis. These stents slowly release medication to prevent tissue accumulation that leads to restenosis. Additionally, between 16% and 50% of people with standard metal stents develop restenosis.
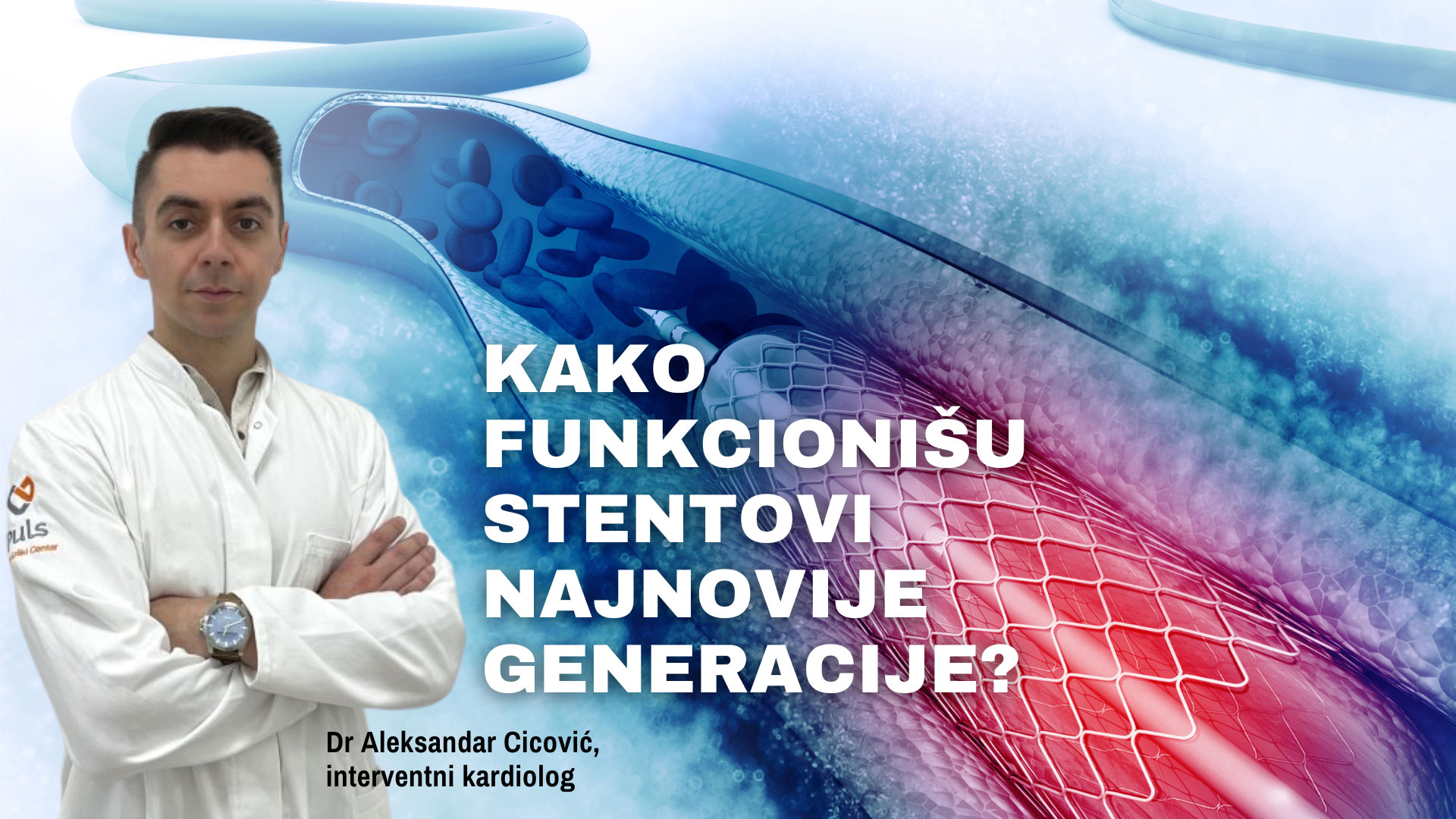
At PULSE Cardiology Center, we use the latest generation of stents with a coating that releases medication against restenosis over several months, making them a long-term solution.
What are the symptoms of restenosis?
The symptoms of restenosis are likely to be similar to the initial symptoms associated with atherosclerosis and may include:
- Irregular or rapid heartbeat
- Chest pain and/or tightness
- Discomfort
- Shortness of breath
- Nausea
- Weakness
- Sweating
What causes restenosis?
There are two main causes of restenosis, one is the growth of scar tissue, and the other is blood clotting at the treatment site.
Restenosis caused by excessive growth of scar tissue: When a stent is initially placed, new tissue forms inside and around it from healthy (endothelial) cells that line the artery wall. This tissue prevents blood clotting as it flows through the stent. However, scar tissue can form underneath the healthy tissue. In about 25 to 30 percent of cases, the growth of tissue beneath the endothelial cell lining can become excessive and obstruct blood flow, creating a new blockage or stenosis (restenosis) around and within the stent.
Blood clotting at the treatment site (thrombosis): The risk of thrombosis is highest immediately after angioplasty, as a result of tissue injury (balloon or metal stent expansion). This form of recurrent narrowing of the blood vessel can be significantly reduced by the use of anticoagulants (blood-thinning medications).
What are the risk factors for restenosis?
You may have a higher risk of developing restenosis if you are older or female. Individuals who have the following conditions are at a higher risk of restenosis:
- Diabetes
- Chronic kidney disease
- Metal allergy
- Multivessel coronary artery disease
- Inflammation caused by the drug from the stent
Treatment of restenosis
There are several different options for treating restenosis that are performed by an interventional cardiologist. The treatment options may include the following procedures:
-Repeat stenting or another stent: If your stent was not properly placed or did not fully expand the blood vessel, the doctor may need to re-expand it using a balloon under high pressure. If the issue is excessive tissue growth, another stent may need to be placed.
-Change of drug in the stent: If you have experienced restenosis more than twice and have a drug-eluting stent, it means that the drug is not preventing the narrowing of the blood vessel. In such cases, the doctor will change the drug in the stent. These drugs help reduce the amount of tissue that accumulates in the artery.
-Bypass graft surgery: This procedure uses healthy blood vessels from other parts of your body to bypass the blocked section of the artery. One end of the blood vessel will be attached below the blockage, and the other end above the blockage..
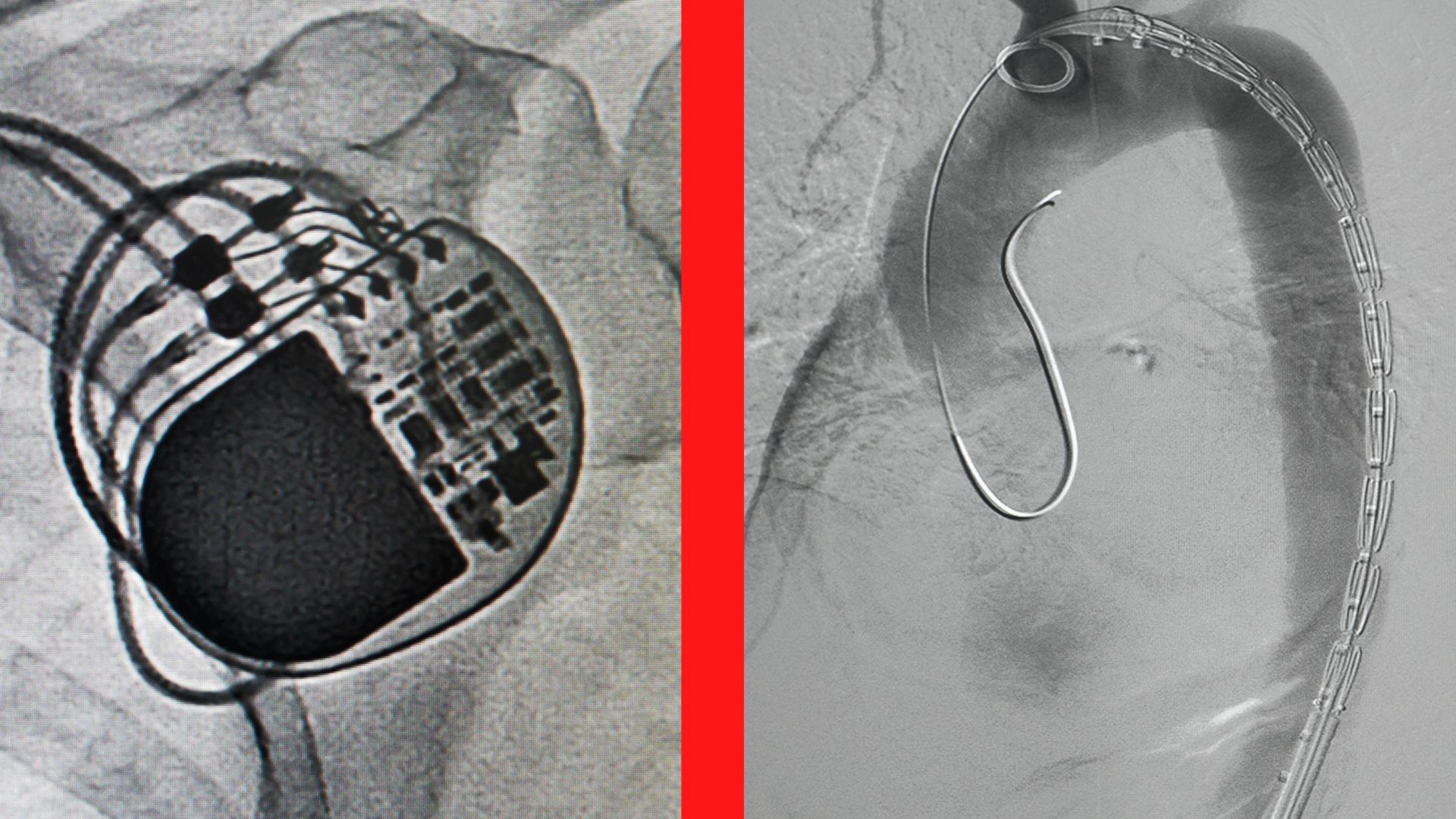
-Coronary angiography and percutaneous coronary intervention: In the case of a blocked blood vessel, an interventional cardiologist can perform cardiac catheterization (coronary angiography), a procedure that allows simultaneous diagnosis and treatment of coronary artery narrowing using a catheter. Once the catheter is in place, one of the procedures for opening the artery is performed: balloon angioplasty or stent placement.
Retrograde approach: This is a specialized technique for treating coronary arteries. It involves redirecting blood vessels around the blockage, utilizing newly formed blood vessels when the artery is severely narrowed.
Cardiac catheterization is performed in a state-of-the-art Cath-lab by experts in interventional cardiology and radiology at the PULSE Cardiology Center.
-Brachytherapy: This is a type of radiation therapy delivered directly inside the artery for about 10 minutes. It can help prevent future tissue growth in the artery, reducing the risk of restenosis.
Preventing the development of restenosis:
All adults, especially those with cardiovascular diseases, should follow the guidelines of world cardiologists to reduce the risk of developing heart diseases, including restenosis. These guidelines address seven risk factors for cardiovascular diseases that individuals can control through lifestyle changes.
- Maintain blood pressure within normal limits. High blood pressure strains your heart, arteries, and kidneys.
- Control your cholesterol levels. High cholesterol leads to plaque buildup that can clog arteries.
- Lower blood sugar levels. High blood sugar can damage your organs.
- Stay physically active. Exercise will help you live longer and improve your quality of life.
- Eat a healthy diet. A heart-healthy diet is one of the most effective ways to prevent and reverse heart diseases.
- Lose weight. Excess weight puts strain on your heart, lungs, skeleton, and blood vessels.
- Quit smoking. Smoking increases the risk of heart diseases